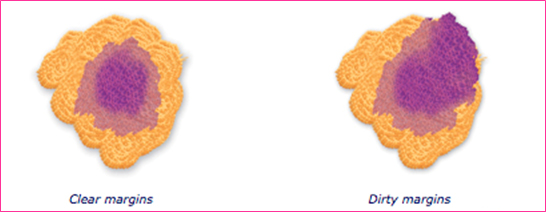
A lumpectomy , or breast conserving surgery, usually removes the least amount of breast tissue. The surgeon removes the cancer and a small portion or margin of the surrounding tissue, but not the breast itself. Even though the lumpectomy is the least invasive breast cancer surgery, it can still be very effective, and further surgery may not be needed as long as the surgical margins are free of cancer cells (clear).
What happens when surgical margins are not clear?
If the final pathology report indicated that one or more or the surgical margins is not clear, or involved by cancer cells, this requires the surgeon to remove a larger portion of the breast than in the lumpectomy to ensure no cancer cells are left behind in the remaining breast tissue.
This can be achieved either by margin re-excision if the remaining breast size is big enough and the margin incolvement is limited, or by moving a whole segment or quadrant of tissue , which requires an Oncoplastic procedure (see Oncoplastic Lumpectomy) to prevent the breast deformity that may result from large simple excision. If the additional procedure did not result in a clear margin for the second time, it means that the disease is more extensive than it appears on radiological examination and the surgeon will offer you a mastectomy — in order to eliminate the cancer.
Types of Lumpectomy
There are different types of lumpectomy depending on weather the tumor is palpable or not, and weather a reconstructive procedure is required with the lumpectomy. Most of the lumpectomy procedures can be done as a day surgical procedure or it may be part of a larger breast cancer operation.
Simple lumpectomy
Also called “wide local excision” because it involved removal of the lump (tumor) with a wider surgical excision of the margins around the tumor. This is usually performed for tumors that the surgeon can feel clinically, and are small in size relative to the breast size so that the procedure would not result in a breast deformity. However, for tumors that are not palpable, another technique should be performed.
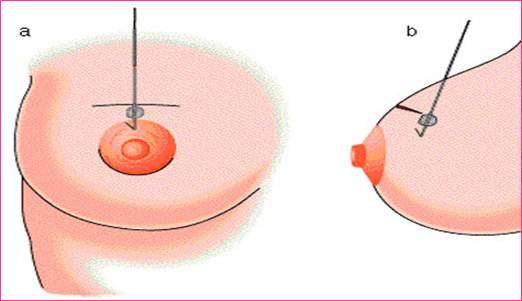
Wire-guided lumpectomy
This is the traditional procedure used for tumors that are not palpable. It is an image- guided procedure performed on two steps, first inserting a small medical wire into the breast tumors guided by an ultrasound or mammogram. This first step is done by the breast radiologist in the radiology department on the morning of the surgery. It is performed under local anesthesia similar to the technique of breast biopsy.
The second step is performed in the operating room, where the surgeon traces this wire to the correct area in the breast that has the tumor, then excises the cancer with a surgical margin.
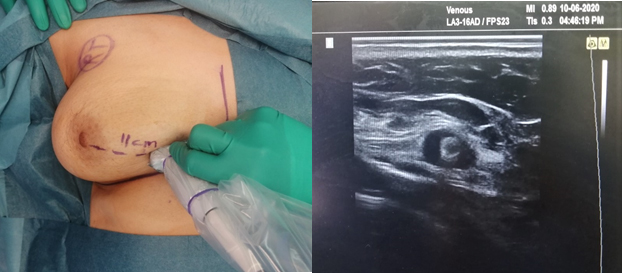
Ultrasound-guided lumpectomy
This is the preferred technique for surgeon who are trained to use the ultrasound machine inside the operating room to identify the non-palpable tumors. It is a one-step procedure that bypasses the wire insertion step, and more convenient to the patient. This technique provides the surgeon with immediate visibility and visual confirmation of the mass being removed. This technique also allows the surgeon to evaluate tumor margins after resection to ensure adequate margins and complete resection.
Research has shown that between 80% and 90% of breast lumps are clearly visible on ultrasound and can be removed using this technique. Many international surgical societies are now recommending for their trainees and members to receive a training course on the use of intraoperative ultrasound.
Dr Jamila Alazhri had a special training during her fellowship in the united stated on the use of ultrasound for the assessment of tumor size, location and surgical planning before surgery, as well as on the ultrasound-guided lumpectomy. She has obtained the ultrasound training certificate from the American Society of Surgical Oncology and the American Society of Breast Surgeons. Dr Azhri has a long experience in performing this procedure and has published related articles.
If you have chosen to undergo a lumpectomy surgery, speak to your surgeon about the feasibility of using this technique. There are some limitations to the use of the ultrasound in few cases where the lesion is not clearly seen by ultrasound, these include calcifications seen on mammogram and lesions seen only by MRI.
Oncoplastic lumpectomy
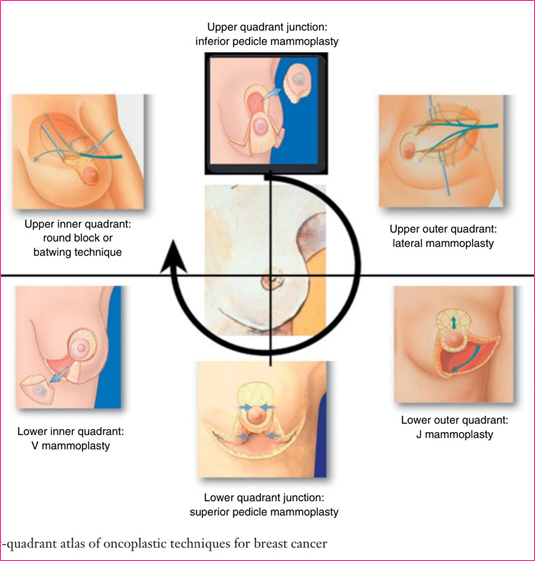
This attractive surgical approach combines traditional breast cancer surgery techniques with the cosmetic advantages of plastic surgery. The goal is to remove the cancerous mass while minimizing the unwanted deformity and effects of surgery and helping the patient recover, both physically and emotionally. The surgeon will remove the tumor through unconventional incisions and use some of the tissues surrounding the tumor to rebuild the missing part of the breast and prevent deformity, especially if the tumor to be removed is large, located in a difficult part of the breast, or the size of the breast is small.
In those situations, the traditional old approach was to perform a mastectomy. However, the introduction of oncoplastic surgery has expanded the scope of breast conserving surgery and enabled great percentage of patients to preserve their breasdts.
There are different levels of oncoplastic surgery. Most of which are performed by a trained breast surgeon. Occasionally a plastic surgeon can join to perform a breast reduction or a lift to make the breasts symmetrical, if the breast surgeon has no experience in this approach.
Dr Jamila Alazhri has an additional training in opcplastic surgery from Paris, France after she completed her Breast surgical oncology fellowship in the United States. She is performing oncoplastic procedures in daily practice since 2016, including procedures like Round-block mastopexy, cresent mastopexy, Bat wing and Hemi-bat wing procedure, J-mammoplasty, V- mammoplasty, theraputic reduction mammoplasty, perforator flap reconstruction, glaandular rotation flaps and more.
She is constantly updating her surgical knowledge and sharpening her skills by attending and participating in international oncoplastic conferences and workshops.