In addition to your surgical procedure, such as a lumpectomy or mastectomy, your doctor may wish to remove and examine lymph nodes to determine whether the cancer has spread and to what extent. Your doctor will use one of two procedures for this, either a sentinel lymph node biopsy/removal or an axillary node dissection. We’ll define these terms below.
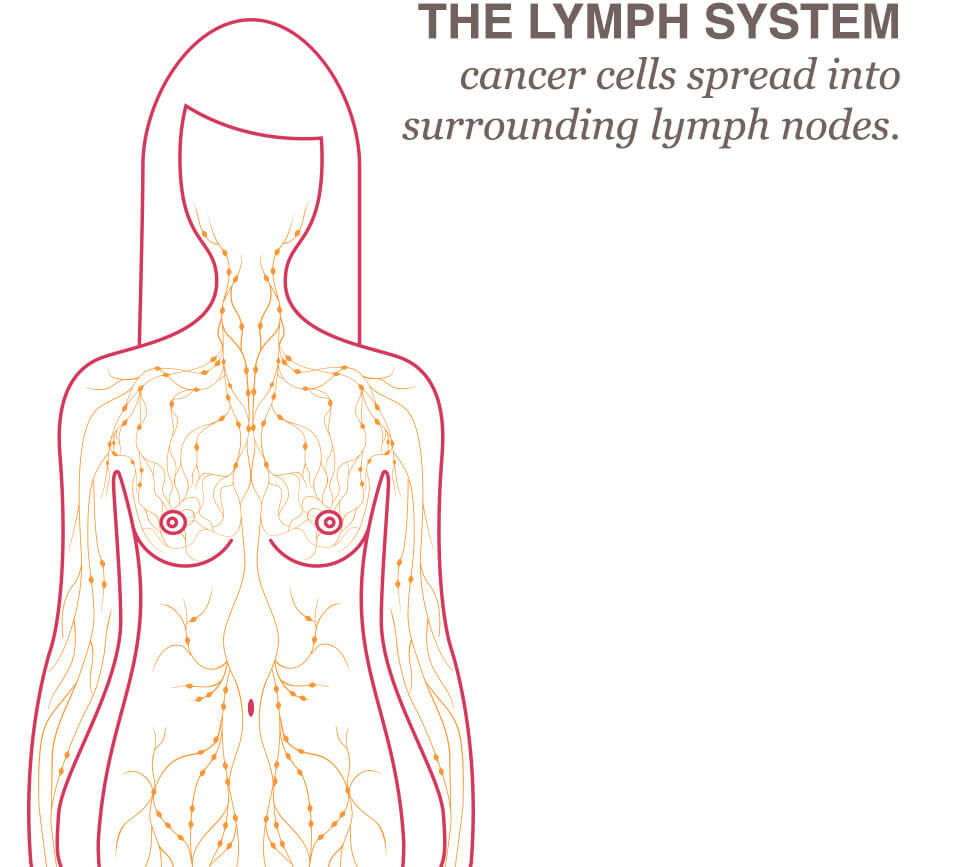
How Does The Lymph System Relate To Breast Cancer?
Although breast cancer is not easily controlled, the spread of breast cancer is sometimes predictable. The cancer cells spread through a customary path, out from the tumor and into the surrounding lymph nodes, before they progress throughout the body.
What is the sentinel node?
The sentinel lymph node (and in some cases there are several grouped together) is the first node “downstream” from the cancer in the lymph circulatory system. If the cancer were to travel away from the breast tumor and into the lymphatic system, this node would be the first one to show evidence of breast cancer.
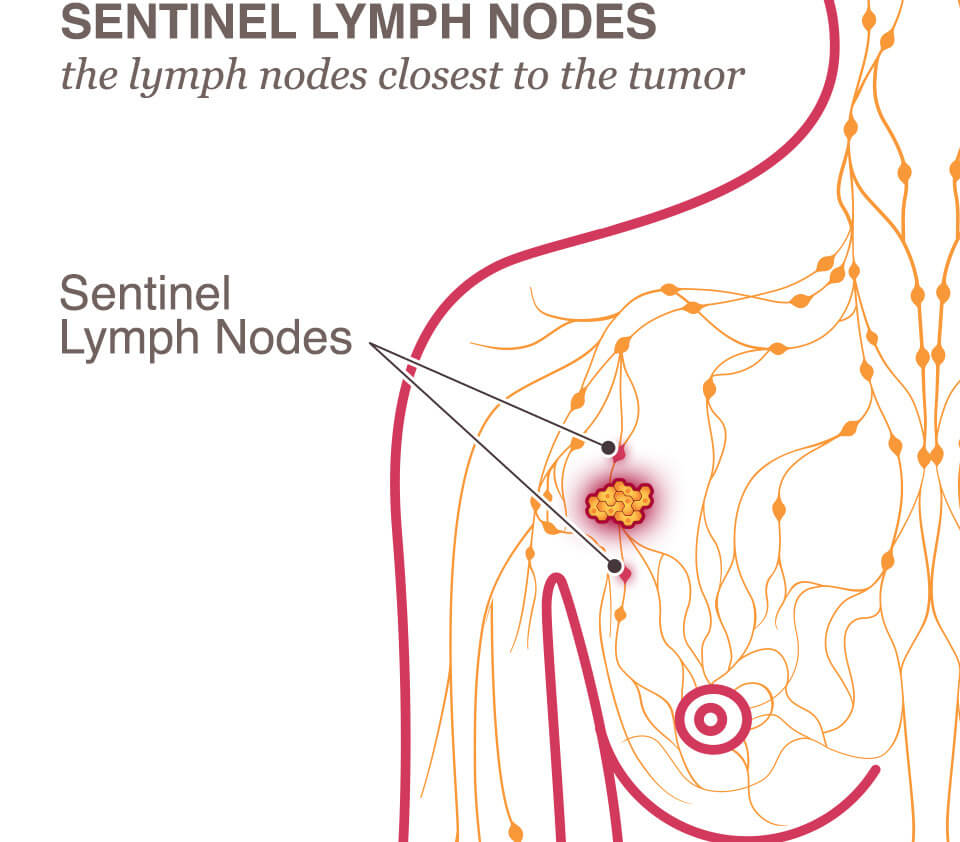
What Is A Sentinel Node Biopsy?
A sentinel lymph node biopsy is a procedure to examine the lymph node closest to the tumor because this is where the cancer cells have most likely spread. First, the surgeon will want to identify the “sentinel lymph node,” the lymph node (or nodes) closest to the tumor. To be able to identify the sentinel lymph node, the surgeon will inject dye or radioactive substances into the tissue near the tumor. The lymph nodes that are the most susceptible to the cancer’s spread will be marked by the dye or radioactive substance. During surgery, the nearest lymph nodes will be removed and checked for the presence of cancer cells.
A biopsy is nearly always taken from the sentinel node, and the breast surgeon typically removes the sentinel node as well for dissection.
What Is An Axillary Node Dissection?
This is a procedure by which the breast surgeon removes some of the axillary lymph nodes, which are the lymph nodes located in the underarm. Once removed, they are dissected and examined.
Do The Lymph Nodes Always Need to Be Removed?
Not always, especially when there is no evidence of any cancer in the lymph system. A mastectomy or lumpectomy operation will most often include either a sentinel node biopsy or an axillary node dissection. Both procedures may be performed through the same or a separate incision.
Axillary node dissection is performed for patients with proven metastasis (spread of cancer) to the lymph nodes (usually by a needle biopsy).
Following sentinel node biopsy, the pathologist will test the lymph nodes to determine whether the cancer has spread past the breast. When some evidence of cancer is found in the lymph system, recent standards are as follows:
- Effective in mid-2012, the standard of care was changed to no longer require women with early stage breast cancers and metastasis to one or two axillary lymph nodes to have a full dissection and removal of the lymph nodes under the arm. Instead radiation to the underarm can be planned.
- For patients with more than 2 diseased lymph nodes, or locally advanced breast cancer (not early), axillary nodal dissection should be performed.
- For patients who received chemotherapy before surgery (neoadjuvant chemotherapy):
- If they had no clinical evidence of nodal disease, sentinel node biopsy can be performed.
- If they had an evidence of nodal disease at the time of surgery, axillary node dissection should be performed.
- If they had an evidence of nodal disease before chemotherapy and it improved after chemotherapy, sentinel node biopsy may be performed using special modified techniques, otherwise, it will not be accurate.
What Is Lymphedema?
Lymphedema is a chronic condition that is caused by a disruption or damage to the normal drainage pattern in the lymph nodes. It most often causes swelling of the arm, but it can also affect the breast. The swelling, caused by an abnormal collection of too much fluid, is called lymphedema. Removing the axillary lymph nodes increases your risk for developing lymphedema.
The risk of developing lymphedema continues for the rest of your life, so it is imperative that you are aware of these risks. Often it is best to learn about preventative measures for lymphedema before surgery so you will know the signs and symptoms to look for and can discuss treatment options with your physician.
After lymph node surgery, if you experience unusual and painful swelling, you should immediately notify your doctor to monitor it. There is no cure for lymphedema, but your doctor can take steps to reduce swelling and maintain that reduction. With proper health care, good nutrition, and exercise, it may be possible for you to reduce the effects of lymphedema. For more information in Arabic, please refer to lymphedema booklet.




